
The Human Cost of America’s Broken Health Care System
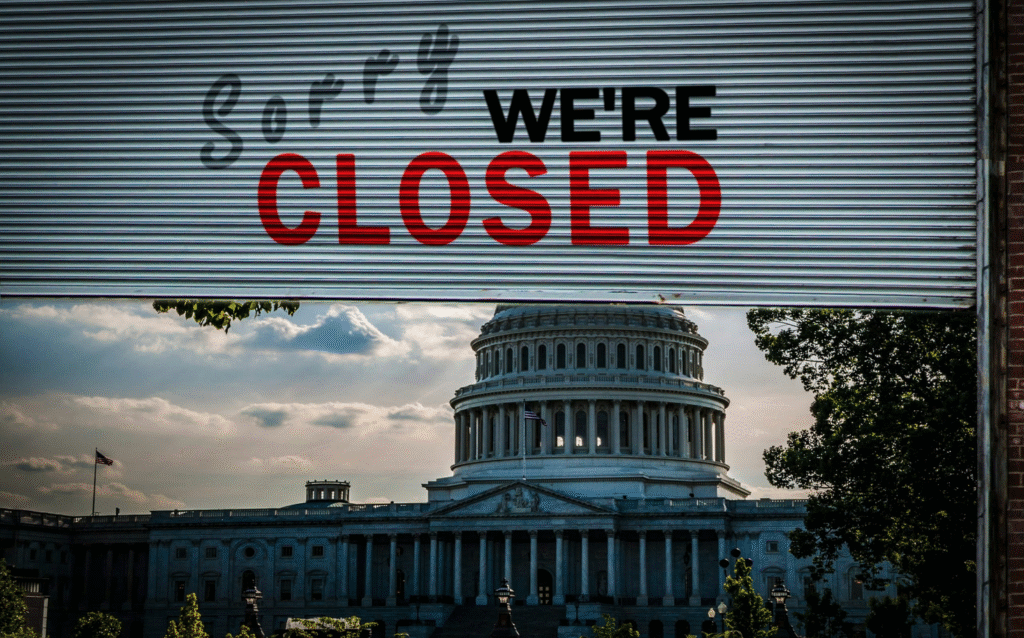
The U.S. health care system spends more per person than any other nation, and yet its outcomes lag behind peers in nearly every key metric. We confront a sobering paradox: high cost without consistently high value.
This is not just a policy issue — it’s a human one. Every woman struggling to get an accurate diagnosis, every patient navigating a fragmented care journey, reflects the cracks in our system. The experience of women with Primary Ovarian Insufficiency (POI) can become a microcosm of what’s wrong — and what’s possible — in U.S. health care.
Why we can’t solve this by simply spending more (or cutting more)
- Chronic underfunding has hollowed out basic public health infrastructure, leaving us poorly prepared for emerging health threats.
- The U.S. system is burdened by administrative bloat, misaligned incentives, overuse, and complexity.
- Patient voices are still often sidelined — research, care pathways, and funding policies frequently prioritize institutional convenience over lived experience.
So, the question isn’t whether to spend more or spend less — the question is how to spend wisely, guided by what actually works for real people.
What a patient-centered, high-impact health model looks like
- Build from lived experience — embed patients as partners in research, care design, outcome selection, and governance.
Example: the newly released Blueprint for Patient-Centered Value Research emphasizes embedding patient perspectives at every stage. - Targeted interventions instead of blanket coverage — not all care needs the same intensity. For POI, we’ve learned that readiness, referral letters, care coordination, and education deliver high impact at relatively low cost.
- Lean infrastructure + smart tech — reduce administrative waste and streamline data flows. Use AI, shared registries, and digital tools to free clinicians’ time for patients.
- Iterative theory-of-change approach — test interventions in small cohorts, measure outcomes, adapt quickly, scale what works. This is the model we propose for POI Readiness™.
What POI teaches us about systemic change
Women with POI often experience delayed diagnosis, fragmented care, lack of clinician awareness, and emotional burden. These challenges arise from systemic failures — but they also point to solutions:
- Early detection matters: the sooner a woman is recognized and treated, the fewer downstream costs and harms.
- Coordination matters: a shared care plan across specialties reduces duplication, gaps, and confusion.
- Empowerment matters: when patients are educated, coached, and given structured tools to advocate, clinical conversations change dramatically.
- Evidence matters: with better registry data and outcome measures, we can justify smart investment instead of waste.
A call to action
If we want a health care system that is patient-centered, effective, and efficient, we must anchor reform in lived experience — not top-down decree. POI Readiness™ is not just a program for women with ovarian insufficiency; it is a testbed for a new way of doing health: Lean, evidence-driven, patient-centered, and scalable.
I invite clinicians, funders, policy makers, technologists, and women with lived experience to join us:
- Help validate and refine the POI Readiness™ model
- Pilot patient-centered research co-design
- Engage in cross-condition thinking: lessons from POI matter for diabetes, mental health, chronic pain, and more
- Advocate for research policies and funding tied to meaningful outcomes
This middle path is not utopian. It is urgent. Let’s close the gap — for women with POI, and for all who deserve a health system that truly works.
For more information see:




